Aging and lifestyle factors increase susceptibility to SARS-CoV-2. A healthy lifestyle may also improve mitochondrial health. Therefore, lifestyle may be crucial in resisting the virus.
RELATED: Epigenetic Modifications — Can Scientists Turn Off SARS-CoV-2?
In this article:
- Lifestyle Increase SARS-CoV-2 Risk
- Mitochondrial Health
- Exercise and Immune Function
- Therapeutic Strategy
Lifestyle Increase SARS-CoV-2 Risk
The risk of severe infection linked to SARS-CoV-2 increases with age and a few other underlying health conditions. As a result, up to 22% of the global population could be at serious risk. Additionally, the higher risk seems linked to an imbalanced or extreme inflammatory response.
The severity of infection may be related to a malfunction in inflammation resolution, resulting in lung hyper-inflammation and cytokine storms.
As we age, the immune system often overreacts to respiratory infections. This overreaction may worsen the response more. An excessive immune response, coupled with age-related loss of adaptive immunity, may correlate to T-cell immunosenescence and thymic atrophy.
Besides, obesity-related conditions, for instance, diabetes, appears to increase the severity of SARS-CoV-2. Because exercise lowers the risk of obesity, it may help prevent viral infection.
Moreover, this suggests that besides aging, lifestyle could determine the likelihood of infection and the severity of the disease.
Researchers argue that a sedentary lifestyle may speed up chronic systemic inflammation related to aging. Besides, there’s a link between obesity pro-inflammatory macrophages and reduced T-cell equilibrium.
On the contrary, exercise is anti-inflammatory, which may explain its benefits. According to some, natural virus hosts, such as bats, have some degree of protection against viruses because they have to find food, and therefore “exercise” frequently.
Mitochondrial Health
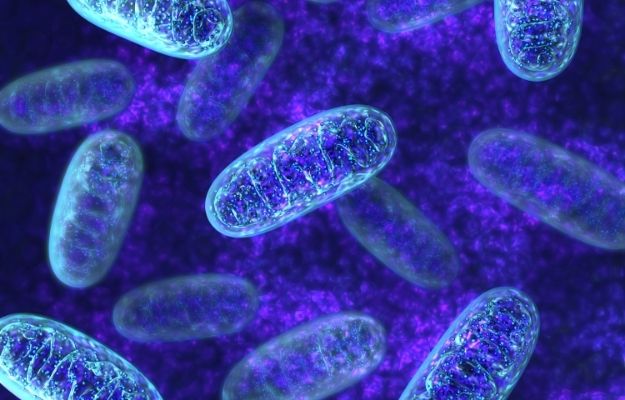
Most cells in the body contain mitochondria, including immune cells. As such, mitochondria are crucial in the body’s immune response. However, viruses alter mitochondria, and for this reason, changes in mitochondrial function may explain some of the variations in SARS-CoV-2 outcomes.
An example highlighting the immune system’s reliance on the mitochondria are those with mitochondrial defects that often display immunodeficiency along with a higher rate of infection.
Besides resisting a virus, the mitochondria may also be relevant in the efficacy of vaccinations. Studies have suggested changes in mitochondrial function may be responsible for the age-related drop in response to influenza vaccines.
In short, changes in mitochondrial function, regardless of age and lifestyle, may impact resistance against infection, as well as the ability to launch an effective response to a vaccine.
Supporting mitochondrial health is crucial, and factors like exercise may add to adequate mitochondrial reserve. This helps the system cope under stress, for example, during a viral infection.
While the virus may only infect specific cells, the immune response is global and reliant on mitochondrial function in various organs and tissues. Notably, scientists associate severity with the hyperinflammatory syndrome, which affects many distinct cell types.
We’ve come to expect this because viruses evolved to manipulate the immune system to hide from it, and this may result in immunosuppression. One example of this is T-cell modulation.
The spike protein of SARS-CoV-2 seems to bind to T-cell receptors (TCRs) and act as a super-antigen. Consequently, the adaptive immune system overreacts, potentially causing the hyperinflammatory syndrome.
RELATED: Epigenetics And Aging: How Some People Are Able To Age Better
Exercise and Immune Function

One can see the effects of hormesis in response to physical exercise, especially aerobic exercise. More specifically, exercise increases mitochondrial function and capacity gradually, regardless of age. Studies suggest those who are physically active not only live longer, but they’re also healthier as they age.
While active muscle is typically inflammatory, it also induces powerful antioxidant and anti-inflammatory mechanisms to offset this. Gradually the adaptive over-compensation creates an enhanced antioxidant and anti-inflammatory feedback, resulting in an overall decrease in inflammation after exercise.
Muscle has other functions, such as supplying and guarding anti-viral stem T-cells. At the same time, it prevents T-cell exhaustion and preserves replication potential during inflammation.
White fat tissue also plays a vital role in adaptive immunity, adding to chronic inflammation. Exercise reduces the volume of fat tissue, and thus inflammation.
Therapeutic Strategy
The immune function relies on mitochondrial function, which declines with age. You can, however, modify the rate of mitochondrial decline through lifestyle.
Mitochondria are central to life. They control many functions, including:
- Energy supply
- Intracellular redox control
- Molecule construction for new growth
- Viruses detection and anti-viral activation
- Regulation of the life and death of the cell
Additionally, mitochondrial health may determine how well an individual will resist a virus and how effective a vaccine will be.
Many viruses, which likely include SARs-CoV-2, change both redox and bioenergetics in the cells they infect for improved replication. Compromised mitochondria function could also induce undue stress in these systems.
These and other findings suggest mitochondrial support could form part of a treatment strategy in patients with severe symptoms.
Lastly, physical activity is one of the crucial elements in mitochondria health and immune function. Therefore, an active lifestyle may help prevent viral infections and reduce severity when infected.
If you’re interested in learning more about epigenetics and research developments, visit the TruDiagnostic website today.
We would love to hear your thoughts about the implications lifestyle and aging have on SARS-CoV-2. Let us know what you think in the comments section!
Source:
Up Next: