Advances in Alzheimer’s disease have been a long time coming. After two decades without new medication, epigenetics is changing our approach, and some of the mysteries surrounding this disease are beginning to open up. We hope to soon gain new insights into ways to end the disease.
RELATED: How To Optimize Brain Health And Longevity With Epigenetics
In this article:
A New Approach To Alzheimer’s Disease
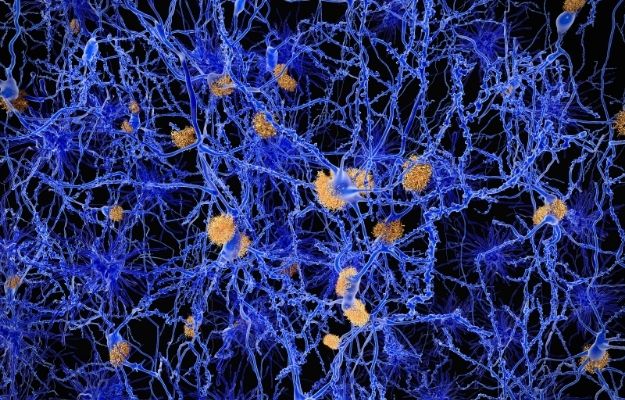
Two proteins in the brain called beta-amyloid plaques and tau tangles, are thought to cause Alzheimer’s disease. As a result, many attempts to treat this illness focused on reducing these proteins. Unfortunately, after hundreds of clinical trials, we still don’t have any new treatments.
Most recently, the FDA voted against recommending aducanumab as Alzheimer’s treatment, despite agreeing that it appears to lessen the proteins thought responsible for the disease. The evidence shows it’s not effective at treating Alzheimer’s.
Perhaps something else is causing the disease, and that’s why the drugs don’t work.
We know there’s a genetic component in Alzheimer’s disease, but we don’t understand it fully. For instance, people who inherit an ApoE gene mutation develop familial or early-onset Alzheimer’s. But not everyone with the mutation develops the disease. Sporadic Alzheimer’s, on the other hand, is more common, and symptoms usually arise after age 65. But the genetic cause is more subtle and divided among many genes.
For this reason, researchers are turning to epigenetics to find answers.
Every cell in the body has the same set of genes, but those genes are selectively active in different cells. Cells have chemical signposts to mark which genes should be activated. Epigenetics is the study of how cells use these chemical signposts.
Additionally, an epigenetic profile can change because of environmental factors or aging, amongst others.
By examining the activated genes in those with Alzheimer’s versus healthy individuals, scientists hope to learn how aging alters the brain and how specific changes cause disease.
So far, researchers have identified notable epigenetic changes connected to Alzheimer’s disease, and we may be able to modify these changes with medications.
Recent Findings
Shelley Berger, from the Epigenetics Institute at the University of Pennsylvania, is studying gene activation in the brain. She’s also looking at patterns of gene activation and how it could link to Alzheimer’s.
Most studies look at cognitively typical samples and Alzheimer’s samples of similar age groups. This choice limits their results to a narrow range of the population.
Berger and her colleagues compared healthy people younger than 65, older individuals without Alzheimer’s disease, and people with Alzheimer’s disease.
By comparing brain cells from three cohorts, they isolated changes that occur naturally with aging that protect and maintain cognition. Moreover, they uncovered that the same protective changes don’t happen in people with Alzheimer’s.
Additionally, they found clues to how gene activation differs in Alzheimer’s disease and healthy aging based on acetyl group placement at different stages.
John Mill and his team from the University of Exeter also looked for epigenetic signals in Alzheimer’s patients by comparing acetyl groups in the DNA from Alzheimer’s brains, as well as healthy brain samples.
They noted in sporadic Alzheimer’s, changes gathered around genes we know are damaged in early-onset Alzheimer’s.
These findings suggest various paths lead to a similar endpoint. For example, with early-onset Alzheimer’s, gene mutation results in dysfunction. But altering gene expression may also cause Alzheimer’s.
However, unlike genetic mutations, epigenetic changes vary throughout a lifetime. The fluidity means it’s possible to alter our epigenetics with medication.
Existing drugs can rearrange the epigenetic signposts in our genome. Whether it can effectively treat Alzheimer’s is the next challenge. We don’t currently know if the epigenetic changes are causing the disease, or if it’s the disease that’s causing changes.
RELATED: Epigenetics And Aging: How Some People Are Able To Age Better
Tau Protein and Epigenetics
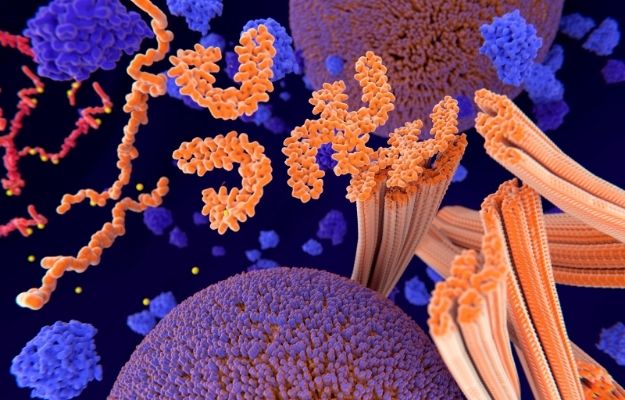
Tau tangles are long strings of protein that collect inside neurons and are distinctive features of Alzheimer’s. Healthy brain cells typically have tau, but in Alzheimer’s, it stops functioning correctly. Instead, it makes tangled masses that ultimately kill the cell.
Philip De Jager and his team from Columbia University in New York studied what epigenetic changes happened when tau tangles are present. While DNA is typically tightly packed, they found tau caused it to become disorganized.
Most importantly, a drug candidate that inhibits Hsp90 protein prevented tau from making these changes. Hsp90 may aid the formation of tau tangles. Blocking it could stop these tangles from forming and prevent the epigenetic changes that follow.
Tau may impact epigenetics. At the same time, epigenetics may also contribute to tau accumulation. It led De Jager and his team to propose that epigenetic changes could impact brain health through the immune system as well.
Immune cells called microglia support neurons by cleaning up cellular debris, preventing beta-amyloid plaques from forming, and aiding brain recovery after a stroke. When tau starts to build up, those microglia become overactive and release chemicals that accelerate tau accumulation.
De Jager’s team tested people who had ApoE mutations but didn’t develop dementia. They had epigenetic factors affecting the activation of genes in the microglia, which appears to reduce the risk of the disease.
Studying the brain comes with unique challenges. As a result, progress towards a cure for Alzheimer’s is slow. A better understanding of how epigenetics affect brain aging and health can potentially unravel the mystery and help scientists find ways to stop this and other age-related brain diseases.
If you’re interested in learning more about epigenetics and research developments, visit the TruDiagnostic website today.
We would love to hear your thoughts about this approach to Alzheimer’s disease. Let us know what you think in the comments section!
Source:
Up Next: